RESEARCHERS ARE USING NON-INVASIVE DEEP BRAIN stimulation techniques (chemogenetics) to activate new brain cells in mice. Remarkably, scientists not only regenerated new cells, but those cells were functional. Today we look at how someday we may use deep brain stimulation for those with Alzheimer’s.
Approximately 32 million people worldwide have Alzheimer’s disease — a dementia type for which there is no cure.
Alzheimer’s disease is a brain disorder that slowly destroys memory and other cognitive skills. We all have memory lapses at times, but the memory loss associated with Alzheimer’s disease progressively worsens over time. The condition ultimately steals away the ability to perform even simple tasks.
For most with Alzheimer’s, symptoms begin later in life. More than six million Americans have the disease, most over age 65. Alzheimer’s disease is the seventh leading cause of death in the USA and is the most common cause of dementia among older adults.
Other dementia forms include Lewy body dementia, frontotemporal disorders, and vascular dementia. Many have mixed dementia — a combination of two or more types of dementia.
“Our novice runs the risk of failure without additional traits: a strong inclination toward originality, a taste for research, and a desire to experience the incomparable gratification associated with the act of discovery itself.”
― Santiago Ramón y Cajal, Advice for a Young Investigator
Chemogenetics: Evolving the lock to fit the key
Chemogenetics involves using inert molecules to alter the activity of brain cells expressing the designer’s receptors. The US National Institutes of Health frames it this way:
“Many patients with nervous system disorders have considerable unmet clinical needs or suffer debilitating drug side effects. A major limitation of existing treatment approaches is that traditional small-molecule pharmacotherapy lacks sufficient specificity to treat many neurological diseases effectively.
Chemogenetics is a new gene therapy technology that targets an engineered receptor to cell types involved in nervous system dysfunction, enabling highly selective drug-controlled neuromodulation.”
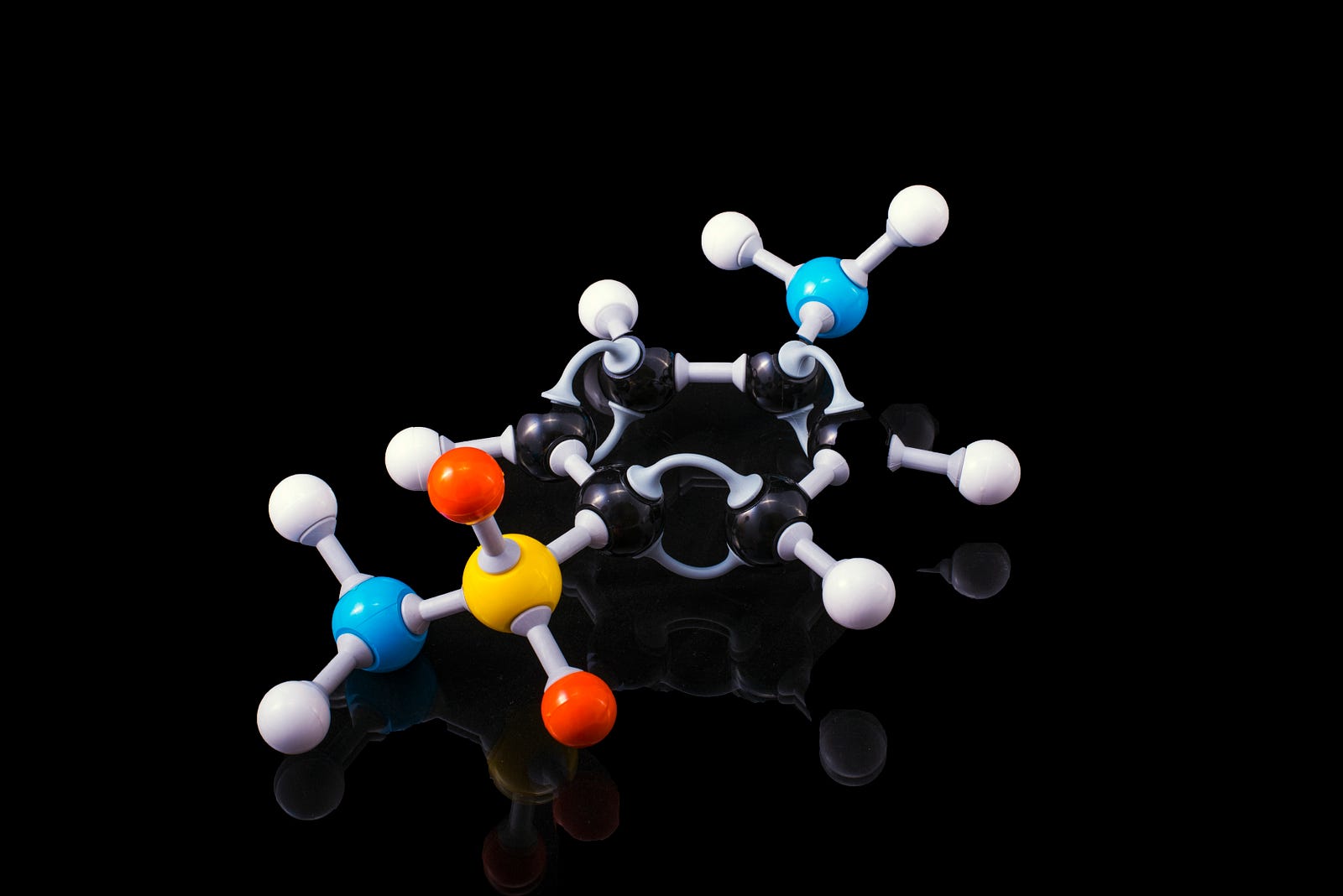
Chemogenetics inverts traditional drug discovery. Historically, scientists developed to target receptors inside cells. On the other hand, chemogenetic approaches determine a clinically approved drug first (based on bioavailability, pharmacokinetics, and tolerability).
Scientists then design a receptor around the drug; the drug is the target! While challenging, protein engineering offers numerous options. They choose the underlying receptor platform based on the following:
- Cellular functional consequences
- The ability to modify it to get varying functional effects
- How simple it is to target with gene therapy.
Using chemogenetics in brain research
In neuroscience, a common experimental approach is to selectively activate (or inhibit) specific nerve subtypes in the brains of model organisms. By doing this, there is gain-of-function (gof) or loss-of-function (lof) in neural circuits.
Chemogenetic activation or silencing of certain nerve cells in the hypothalamus dramatically increases (or decreases) food intake. Perturbing nearby cells impacts sex, aggression, emotions, sociality, and thermoregulation in mice.
In summary, chemogenetics generalizes chemical control of cell pathways by engineering tunable and modular systems that target selected receptors. Investigators can install the systems in virtually any cell population. Chemogenetics allows for impressive selectivity of cell type-specific evaluation of brain functions.
What is deep brain stimulation?
Deep brain stimulation is a surgical procedure in which a surgeon places electrodes in a specific brain area. The electrodes are attached, via wires, to a small pacemaker-like device placed under the chest skin.
The electrodes create electrical pulses that override abnormal signals that can cause neurological problems. There has recently been a move to develop less invasive deep brain stimulation methods.

The Mayo Clinic explains that medical teams use deep brain stimulation to treat several conditions, including the following:
- Parkinson’s disease
- Essential tremor
- Dystonia
- Epilepsy
- Obsessive-compulsive disorder
Scientists are studying deep brain stimulation as a potential management tool for:
- Tourette syndrome
- Huntington’s disease and chorea
- Chronic pain
- Cluster headache
Historical research has examined deep brain stimulation as a potential treatment for Alzheimer’s.
Creating new nerve cells in brains with Alzheimer’s
University of North Carolina at Chapel Hill (USA) researchers recently created new nerve cells (neurons) in the brain, triggering them with deep brain stimulation. The mice with dementia subsequently had better cognitive and non-cognitive functioning.
For the initial study phase, Juan Song, Ph.D., and colleagues used optogenetics to stimulate a brain region linked to memory in Alzheimer’s mice. This approach generated new neurons in the brains of the mice with Alzheimer’s.

Listen to Dr. Song explain:
“In adult human brains, the hippocampus generates new neurons (adult-born neurons, or ABNs) across age. ABNs help us maintain memories and regulate emotions. In people with Alzheimer’s disease, this process is impaired. To achieve symptom relief, ABNs are a potential target.”
Increasing neuron activation
Next, Dr. Song and colleagues used a non-invasive deep brain stimulation approach (chemogenetics) to activate the new nerve cells. The researchers used inert molecules to change the activity of neurons expressing receptor targets.
The chemogenetic approach increased the activity of adult-born neurons, nerves that appear to be related to cognitive and non-cognitive symptoms in Alzheimer’s disease mouse models. Dr. Song explains:
“Chemogenetics involves using inert molecules to alter the activity of brain cells expressing designer’s receptors. We used chemogenetics to increase the activity of SuM-enhanced ABNs, which appears to be critical for their beneficial effects on both cognitive and non-cognitive symptoms.”
Activation of the adult-born neurons (ABNs) restored cognitive and affective deficits in Alzheimer’s mouse models.
Alzheimer’s disease treatment potential
The current study is promising. Hopefully, we will see the promising results translate well to humans. The researchers look forward to identifying genes and pathways mediated by the activation of adult-born neurons.
Ultimately, researchers hope to develop first-in-class, exquisitely targeted therapies to treat Alzheimer’s and other dementia types. I will end with some ways that you may reduce your risk of dementia:
5 Simple Ways to Drop Your Dementia Risk
WHILE THERE IS NO CURE FOR ALZHEIMER’S DISEASE, there are some lifestyle moves you can make that may lower your risk of…medium.com
If you know someone with breast cancer, here is my comprehensive online course:
Dr. Michael Hunter’s Wellness!
Edit descriptionbreastcancerbydrhunter.thinkific.com
Join Medium with my referral link – Michael Hunter, MD
Read every story from Michael Hunter, MD (and thousands of other writers on Medium). medium.com
Get an email whenever Dr. Michael Hunter publishes.
Get an email whenever Dr. Michael Hunter publishes. drmichaelhunter.medium.com
The information I provided in this blog is for educational purposes only and does not substitute for professional medical advice. Please consult a medical professional or healthcare provider for medical advice, diagnoses, or treatment. I am not liable for risks or issues associated with using or acting upon the information in this blog.
Thank you for reading “Brain Stimulation for Alzheimer’s.”




