FOR THOSE DEALING WITH OBESITY, LOSING WEIGHT through intermittent fasting has fascinating effects on the brain-gut-microbiome axis. Today, we explore the connection between the gut and the brain.
A new small study shows intermittent energy restriction can lead to brain changes that make you less inclined to overeat. Moreover, the approach can boost the variety of gut microorganisms.
Today, we explore how the gut microbiome communicates with the brain in a complex, two-directional way. First, we’ll explore the microbiome before turning to intermittent timed feeding (fasting).
Finally, we’ll look at a new study that shows a weight-influencing bidirectional relationship between the brain and the gut.
Microbiome
Here’s what I previously wrote in Medium about the microbiome:
The microbiome is the vast and diverse community of microbes living within and on the body.
The term encompasses viruses, bacteria, fungi, and other microscopic organisms that harmonize with our cells.
These microorganisms play a vital role in maintaining our health and overall well-being.
Most of the microbiome resides in our gut, although it also inhabits other body parts, such as the skin, mouth, and reproductive organs.
The microbiome is incredibly complex and consists of trillions of microbial cells, collectively outnumbering our human cells.
These microorganisms have coevolved with us over millions of years, establishing a mutually beneficial relationship.
Microbes help in essential functions such as digestion, nutrient absorption, and immune system development, and they even influence our mood and behavior.
Intermittent energy restriction (IER)
First, let’s define IER.
Intermittent energy restriction (IER) refers to eating patterns in which individuals go through short periods of restricted food intake, alternating with periods of unrestricted food intake.
There are many variations of intermittent energy restriction diets. Examples include the following:
- alternate-day fasting (ADF)
- time-restricted feeding (TRF).
Long-term intermittent energy restriction can be an effective method for weight loss.
Periodic fasting
Periodic fasting involves calorie restriction (or complete fasting) for 48 hours to a week or longer.
Periodic fasting is usually practiced far less frequently than intermittent fasting (rarely more than once every two weeks).
It is sometimes carried out “as needed” rather than at specific intervals.

Two main periodic fasting approaches are:
- Prolonged fasting: Total fasting for an extended period, often three days or longer.
- Fasting-mimicking diet (FMD): A diet with similar metabolic effects to fasting, with 30–50% reduced calorie intake for four to seven days.
Since water-only fasting is difficult to sustain, folks have developed other dietary regimens that mimic the effects of fasting.
These alternative approaches do not require complete eating abstinence for an extended time.
Study
In a Chinese study, 25 obese individuals lost weight after a two-month intermittent energy restriction intervention.
Researchers used functional MRI to analyze the activity of specific brain regions.
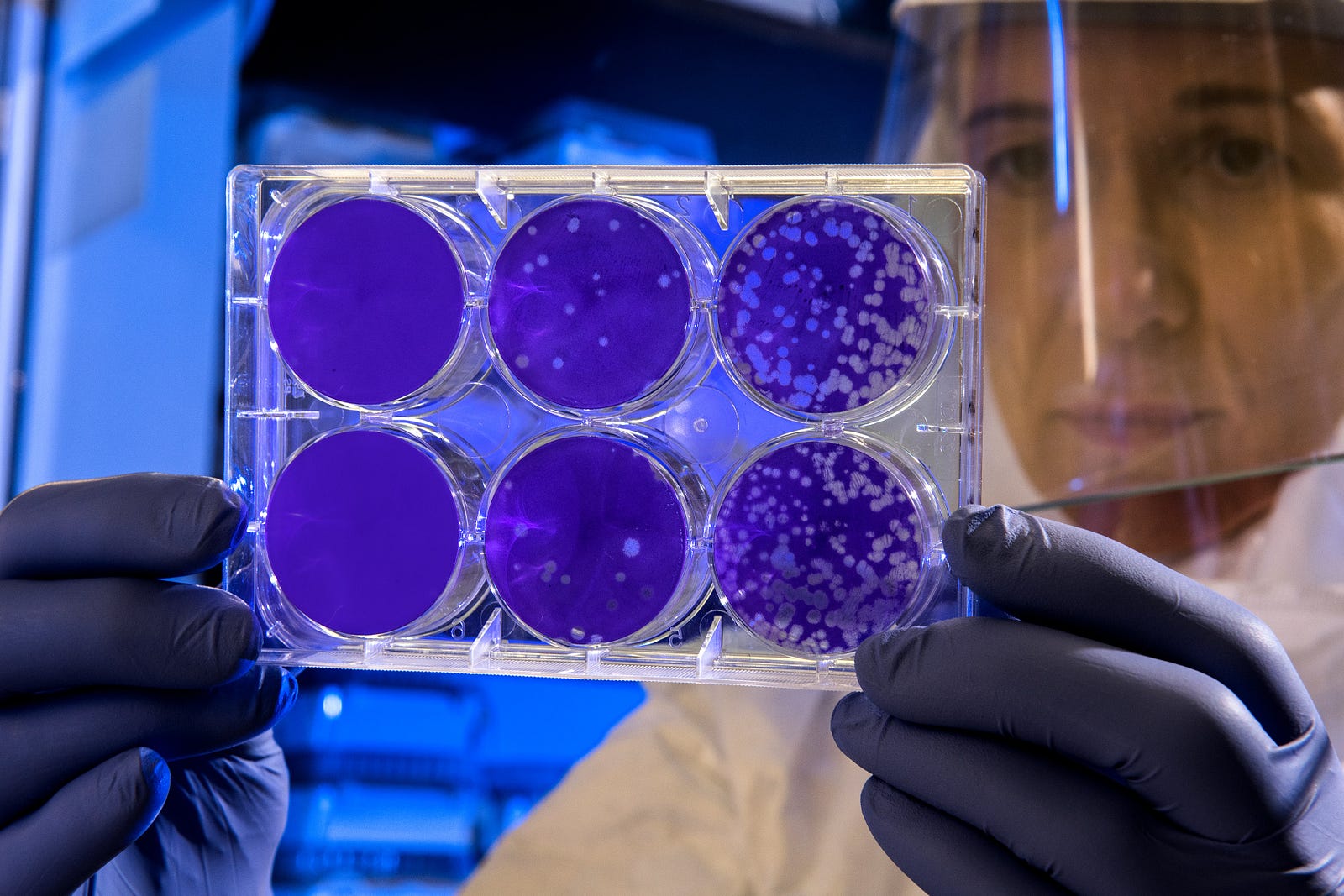
They also did metagenomic sequencing to identify gut microbes in fecal samples.
This next-generation sequencing approach is one of several high-throughput sequencing methods that simultaneously sequence billions of nucleic acid (substances in our DNA, RNA, and more) fragments.
Results
Intermittent energy restriction reduced obesity-related brain region activity.
Moreover, the diet approach also reduced the number of E. coli bacteria across multiple time points.
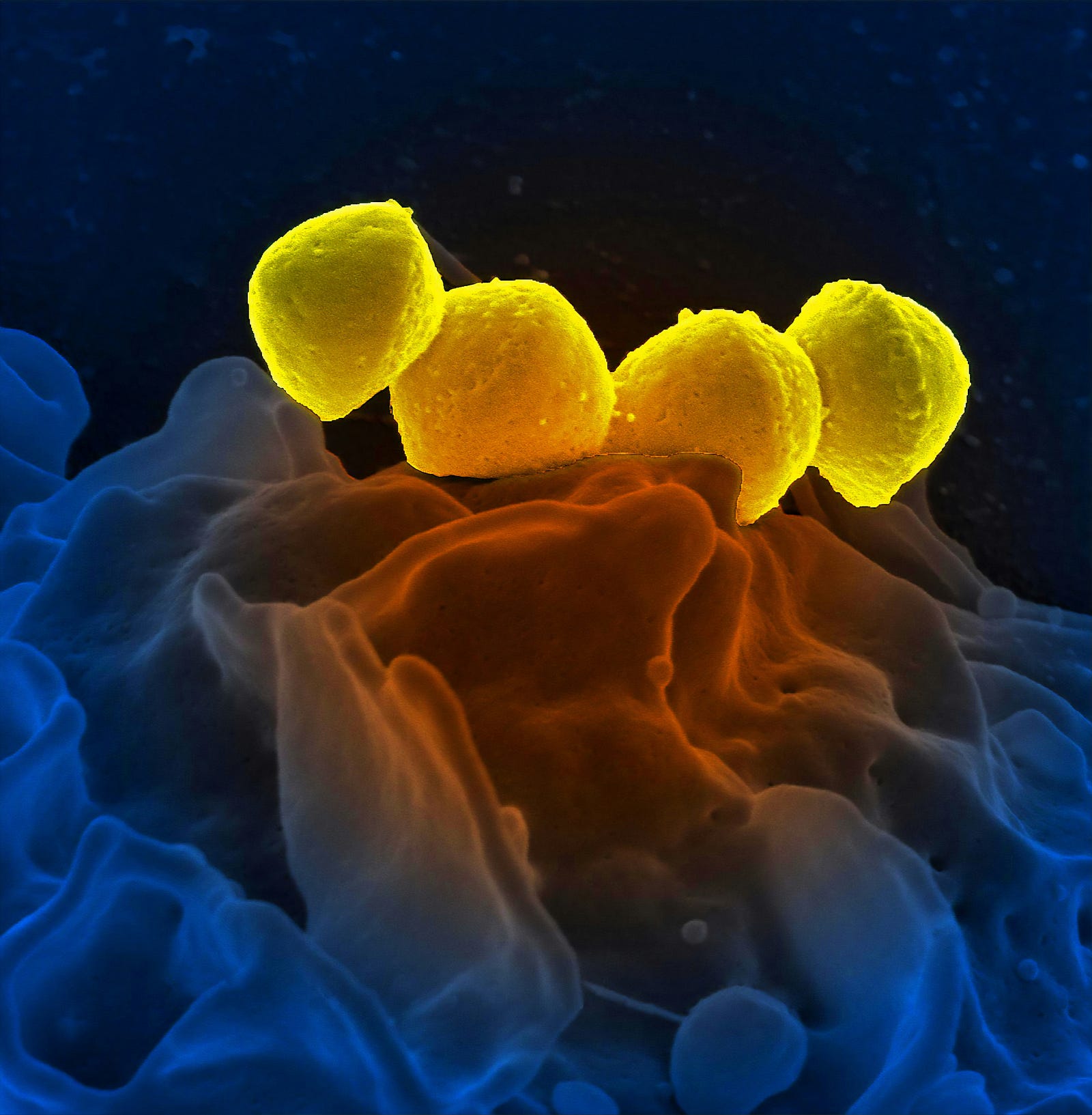
It also elevated the abundance of obesity-related bacteria (Faecalibacterium prausnitzii, Parabacteroides distasonis, and Bacterokles uniforms).
Analysis revealed correlations between gut bacteria abundance alterations and brain activity changes.
My take — The Gut and Brain
The researchers performed their last measurements 30 days after the eating intervention.
We need a long follow-up to understand the dynamic alteration of the brain-gut microbiome affecting long-term weight loss.
While the scientists could not establish a causal relationship, they provided insights about the relationship between certain brain area activity and specific gut flora in weight loss.

The blood-gut microbiome axis has plasticity in adults, helping to regulate food intake and keeping our weight stable.
The gut microbiota creates chemical signals that determine eating behavior through interactions with the brain.
Thank you for reading “The Gut and Brain.”




