IN THE EVER-EVOLVING HEALTHCARE LANDSCAPE, staying up-to-date with the latest guidance on cancer screenings can be central to your well-being. Today’s topic is Navigating Cancer Screenings: Stay Updated with the Latest Guidelines.
I want to give you a cancer screening roadmap that might help you detect potential issues early on when they’re most manageable.
Imagine cancer screenings as preventive pit stops that can steer you away from health hazards, ensuring a smoother ride toward a healthier future.
I’ll break down the latest guidelines, making it easy to navigate the who, what, when, where, and why of these screenings.
So, buckle up as we embark on a journey to empower you with the knowledge needed to take charge of your health and well-being.
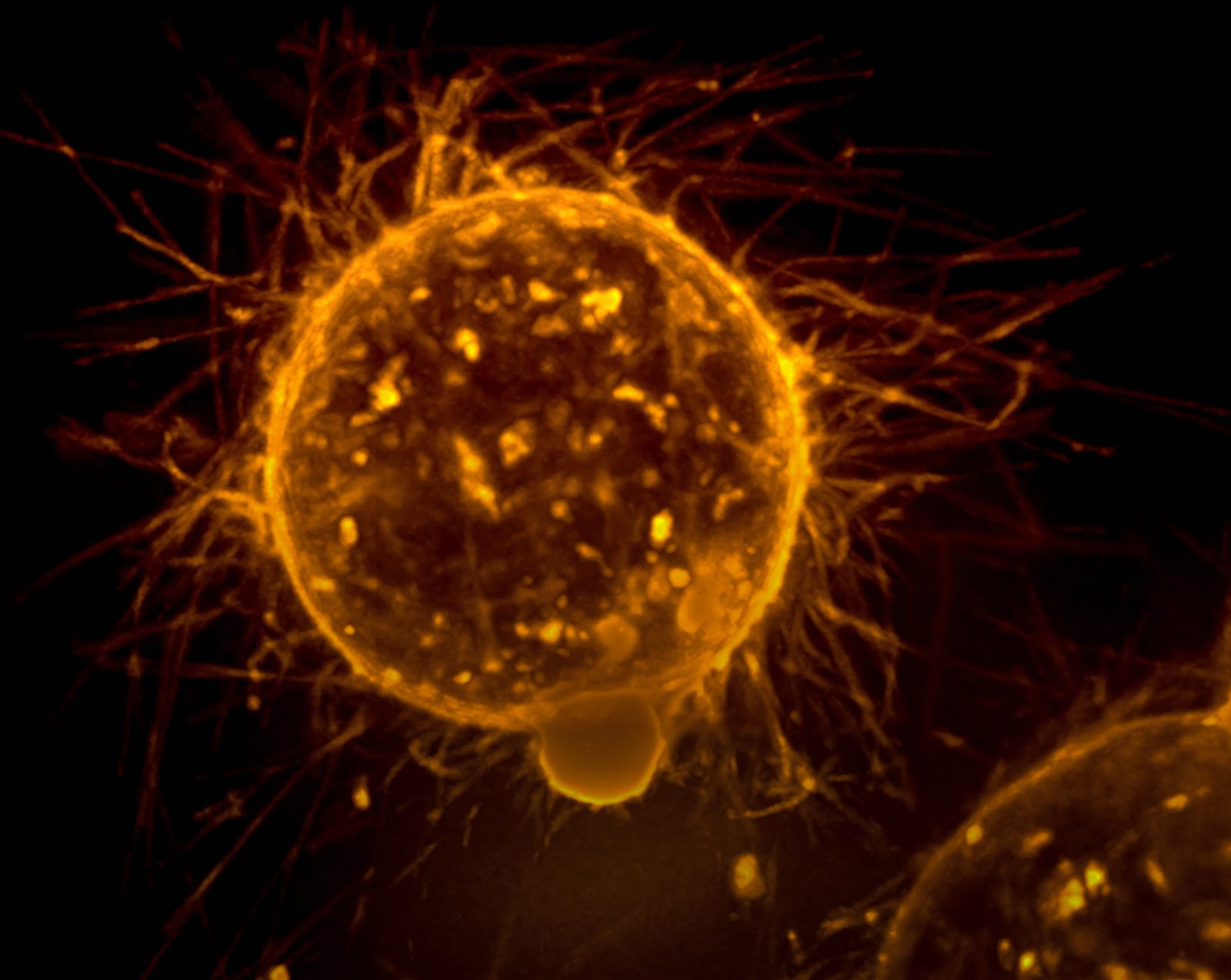
1. Breast cancer screening (females)
I am a radiation oncologist with a special interest in breast cancer. I am always surprised at how there are several differing guidelines for breast cancer screening.

Here is what I recommend, as advocated by the U.S. Preventative Services Task Force (USPSTF) in its recent draft guidance:
- Women (at average risk) as young as 40 should get checked for breast cancer every two years. This age is ten years lower than what the USPSTG historically suggested.
- While the USPSTF recommends that women 40 to 74 consider screening every other year, other expert groups advocate for annual screening.
- Medical groups also disagree on when women should stop getting mammograms. The task force said women should discontinue screening at age 75.
Why did breast cancer screening guidelines change?
The American College of Radiology reminds us that one in six breast cancers occur in women in their 40s.
The organization also notes that mammography screening cuts the risk of dying from breast cancer nearly in half.

Finally, three out of four women diagnosed with breast cancer have no family history of the disease and are not considered high-risk.
“Women in their 40s are developing breast cancer more than ever before,” said John Wong, MD, a member of the task force and chief of the division of clinical decision-making at Tufts Medical Center (USA).
Additional imaging
Certain organizations and healthcare facilities suggest that women with denser breasts consider undergoing extra screenings such as ultrasounds or MRIs.
However, insufficient evidence supports or opposes this practice, and insurance coverage for these additional screenings is inconsistent.
The American College of Radiology recommends that women engage in discussions with their healthcare providers by the age of 25 to determine if they may be at a heightened risk of breast cancer before opting for any screening procedures.
The U.S. Preventative Task Force said there was not sufficient evidence on screening women 75 and older or to recommend whether women with dense breast tissue should get additional screening testing.
Women over 75 should consult with their doctor about whether to discontinue breast cancer screening.
High-risk
Women with a cumulative lifetime breast risk of at least 20 percent are considered high-risk.
The drop in first mammogram age to 40 is especially important for Black women. These gals are more likely to develop aggressive cancers at young ages.

Moreover, Black women are 1.4 times more likely to die from breast cancer than whites, despite similar screening rates.
Compared to average-risk women, elevated-risk women are more likely to be diagnosed with larger breast cancers, node-positive cancers, and interval cancers.
All of these cancers are associated with worse prognoses.
Breast cancer screening harms
But screening also comes with downsides, which include the risk of overdiagnosis and overtreatment.
A recent study suggests that the overdiagnosis risk with routine screening mammograms is substantial for women in their 70s and older.
2. Colorectal cancer screening
As an oncologist, colorectal screening is important for several reasons.
First, screening helps detect colorectal cancer early when treatment is more effective (and the chances of successful recovery are higher).
Early detection can also prevent the development of advanced and potentially more challenging-to-treat stages of colorectal cancer.

Screening can detect pre-cancerous polyps.
Colorectal cancer often develops from pre-cancerous polyps, and screening allows for the identification and removal of these polyps before they become cancerous.
This preventive measure significantly reduces the risk of colorectal cancer development.
Regular screening is essential because symptoms of colorectal cancer may not manifest until the disease has progressed.
Screening enables the detection of abnormalities or cancerous changes in the colon or rectum before symptoms like bleeding or changes in bowel habits become noticeable.
Ultimately, colorectal cancer screening plays a crucial role in promoting early detection, prevention, and overall better outcomes in the fight against colorectal cancer.
Colon cancer screening guidelines
The U.S. Preventative Services Task Force suggests this:
Individuals at average risk should start colorectal cancer screening at age 45.
This age represents a drop from a starting age of 50 a few years ago.
This age represents a drop from a starting age of 50 a few years ago.
Screening should continue until age 75, according to the task force, after which it depends on the individual patient and their doctor until age 85.
Why did colon cancer screening guidelines change?
The U.S. Preventive Services Task Force (USPSTF) concludes with high certainty that screening for colorectal cancer in adults aged 50 to 75 years has substantial net benefit. The guidelines (from 2016) stayed the same for this age bracket.
The USPSTF concludes with moderate certainty that screening for colorectal cancer in adults aged 45 to 49 years has moderate net benefit. The USPSTF dropped the start age from 50 to 45.
In the past decades, the incidence of colorectal cancer (CRC) in people under the age of 50 years has increased.
Colorectal cancer before 50 is early-onset CRC or young-onset CRC (YO-CRC).
Colorectal screening for older individuals
The USPSTF concludes with moderate certainty that screening for colorectal cancer in adults aged 76 to 85 years who have had previous screening has a small net benefit.
Colorectal screening should continue until age 75, according to the task force, after which it depends on the individual patient and their doctor until age 85.

In general, adults (of any age) who have never had screening for colorectal cancer are more likely to benefit.
Colorectal screening frequency
How often you get screened depends on the test.
For stool tests, including the ones that can be done at home, individuals should have screening every one to three years.
Repeated studies should be done once every ten years for those who do not have an increased risk of colorectal cancer). Doctors can remove pre-cancerous polyps during that exam.
Colorectal screening harms
No studies reported on harms from stool-based tests.
The risks from stool-based screening tests come from false-positive and false-negative results and harms of the workup of positive screening results, such as colonoscopy.
Serious side effects from colonoscopy to follow-up positive screening results are estimated to be 17.5 serious bleeding events and 5.4 perforations per 10,000 colonoscopies.9,10

Screening colonoscopy can cause the following harms:
- Serious bleeding (around 15 events per 10,000 colonoscopies)
- Perforations (around three events per 10,000 colonoscopies)
- Cardiopulmonary events (rare, but frequency not clear)
- Other (including infection and other gastrointestinal events)
3. Lung cancer screening
Do you have a history of smoking cigarettes?
Expert groups suggest you may be a candidate for annual low-dose C.T. scans for lung cancer screening.
Lung cancer is one of the most common and deadly cancers in the United States.
Although lung cancer death rates have decreased in recent years, there are significant disparities by sex and race/ethnicity.
Screening and interventions to prevent tobacco initiation and help people quit smoking can help lower the number of lung cancer deaths.
Lung cancer screening details
You are a candidate for lung cancer screening if you fit all of these criteria:
- You are 50 to 80 years old.
- You have a cigarette smoking history of at least 20 pack-years (for example, one pack per day for 20 years or two packs per day for ten years).
- You currently smoke (or quit within the last 15 years).

The expert panel suggests that those meeting these criteria engage in shared decision-making (examining the potential benefits and risks of screening) with their healthcare provider.
Lung cancer screening frequency
If you decide to do lung cancer screening, you will ideally go to a center with expertise in lung cancer screening.
If you smoke, you should have interventions to help you quit.
Screening consists of annual lung C.T. (“cat”) scans.
In general, screening should stop once a person has not smoked for 15 years or has a health problem that limits life expectancy.
4. Prostate cancer screening (males)
The prostate-specific antigen (PSA) blood test looks for prostate cancer signs. Such screening can help find cancer early, then treatment is most effective.
For many, getting a PSA is a good idea. However, prostate cancer screening has pros and cons. First, the upsides:
- Prostate cancer screening may help you detect cancer early. Cancer is easier to manage and more likely to be cured early.
- PSA testing uses a simple, widely available blood test.
- The number of prostate cancer deaths has gone down since PSA testing became available.
Prostate cancer screening: Who?
Most expert cancer organizations encourage men in their 50s (with a life expectancy of at least ten years) to review the pros and cons of prostate cancer screening with their healthcare professionals.

Some may consider starting earlier than 50:
- Age 45 for men at high risk of developing prostate cancer. The high-risk category includes African American men and men who have a first-degree relative (father or brother) diagnosed with prostate cancer at an early age (younger than age 65).
- Age 40 for men at even higher risk (those with more than one first-degree relative who had prostate cancer at an early age).
If you choose to have prostate cancer screening, most organizations recommend stopping around age 70 or if you develop other serious medical conditions that limit your life expectancy.
Prostate cancer screening: Frequency
According to the American Cancer Society, If screening reveals no prostate cancer, the time between future screenings depends on the results of the PSA blood test:
- Men with a PSA of less than 2.5 ng/mL may only need retesting every two years.
- Screening should be done yearly for men whose PSA level is 2.5 ng/mL or higher.
Prostate cancer screening downsides
Now, the downsides:
- Some prostate cancers slowly grow and never spread beyond the prostate gland.
- Not all prostate cancers need treatment. Treatment for prostate cancer may have risks and side effects, including urinary incontinence, erectile dysfunction, or bowel dysfunction.
- PSA tests aren’t foolproof. Your PSA levels can be high when cancer isn’t present and normal when cancer is present.
- A prostate cancer diagnosis can provoke confusion and anxiety. Concern that the cancer may not be life-threatening can make decision-making complicated.
- False negatives: Sometimes, prostate cancer does not make PSA.
Ultimately, whether to have prostate cancer screening is something you should decide after discussing it with your healthcare provider, considering your risk factors, and weighing your personal preferences.
5. Cervix cancer screening (females)
The U.S. Preventive Services Task Force (USPSTF) recommends:
- Women 21 to 65: Screen with cytology (Pap smear) every three years.
- Women 30 to 65: Screen with cytology (Pap smear) every three years or co-testing (cytology/HPV testing) every five years.

Cervix cancer risk factors include the following:
Human papillomavirus (HPV) infection is linked with almost all cervix cancers. Other risk factors that put a woman at increased risk of cervical cancer include:
- HIV infection
- Compromised immune system
- In utero exposure to diethylstilbestrol (DES)
- Previous treatment of a high-grade pre-cancerous lesion or cervix cancer.
Summary
Cancer screening aims to identify cancer before a person has symptoms. We reviewed several screening tests and recognized that they each have risks.
Moreover, false positives (the test indicates there is cancer when there is not) and false negatives (the test indicates there is no cancer when cancer is present) can occur.
Finding cancer may not always improve an individual’s health or help you to live longer. Understanding the benefits and risks of screening tests is critical to deciding which tests are right for you.
Nevertheless, the appropriate cancer screening saves lives.
Selected high-risk individuals (for example, with a “breast cancer gene” such as BRCA1 or 2) may have additional screening interventions.
Get an email whenever Dr. Michael Hunter publishes.
drmichaelhunter.medium.com.
Thank you for reading “Cancer Screening.”




