Is the Appendix Useless? I remember the call from when I worked in Seattle. My 10-year-old daughter was in the emergency department in Portland, Oregon.
No problem, I thought.
Get the appendix out.
I know, I know.
While appendicitis can be a time-sensitive condition due to the risk of rupture, a randomized clinical trial suggests antibiotics might offer an alternative to surgery (appendectomy) for uncomplicated cases.
However, surgery remains the standard approach in the United States.
Nina didn’t need her appendix, right? It’s a vestigial organ without function, isn’t it?
For over a century, the appendix has been relegated to the realm of the “useless organs,” destined for removal with little fanfare.

But recent scientific discoveries are casting doubt on this long-held belief. In the grand court of human anatomy, the appendix is finally getting its day.
Was I Wrong?
New research suggests this enigmatic organ might be more crucial than previously thought.
Join us as we delve into the fascinating world of the appendix, exploring the latest findings that challenge our understanding of this once-dismissed body part.
Is the appendix a medical enigma or a hidden champion of our health?
Let’s unveil the evidence and see if the appendix can be vindicated.
New Thinking – Is the Appendix Useless?
I might need to adjust my view that the appendix is a useless leftover.
New research suggests it might be a helpful companion in our belly.

Let me put it differently: Think of it as a cozy apartment for good gut bacteria and a training ground for our immune system to fight off invaders.
It might even be linked to some health conditions, like ulcerative colitis and even Parkinson’s disease.
This observation is interesting news for the 300,000 Americans who get their appendix removed each year.
However, there’s a catch: scientists are still figuring out when the appendix is a hero and when it might be better off gone.
New Research: The Appendix Is Not Useless
The most heated scientific discussion surrounds the links between the appendix and conditions such as Parkinson’s disease, ulcerative colitis, and colorectal cancer.
For example, a small 2019 study showed that removing an appendectomy — appendix removal — may improve symptoms of certain forms of inflammatory bowel disease that are resistant to standard medical treatments.
A third of patients with ulcerative colitis improved after removing their appendix, and 17 percent fully recovered.

Why?
An appendectomy may work for ulcerative colitis because it suppresses the immune system, especially in the lower intestinal areas.
A 2023 meta-analysis found that people who had their appendix removed before being diagnosed with ulcerative colitis were less likely to need their colon removed later on.
Parkinson’s Disease
For years, Parkinson’s disease (PD) was like a detective story focused solely on the brain.
But recent studies throw a wrench in that theory, suggesting the culprit might lurk in our gut.
Enter the surprising suspect: the appendix.
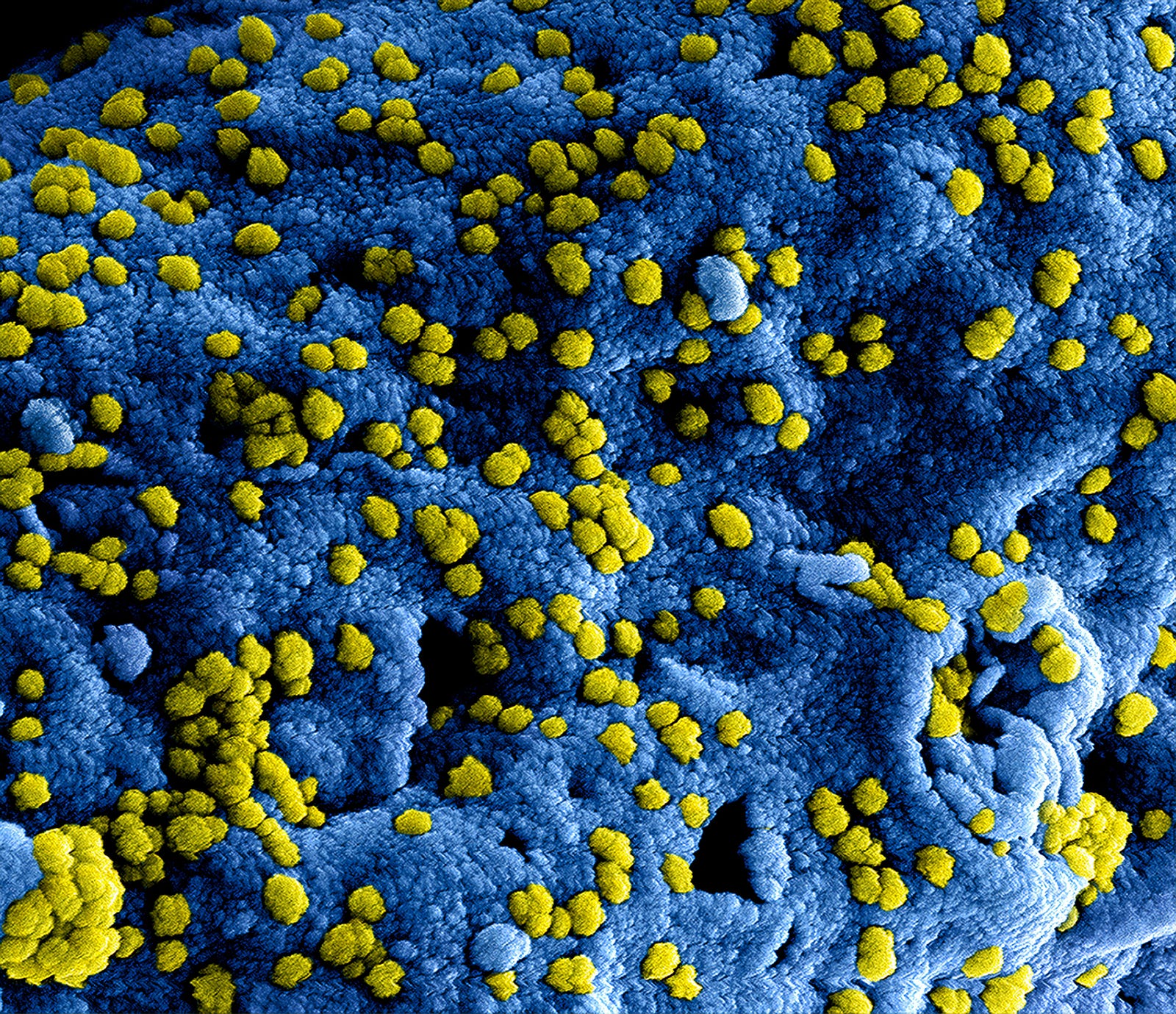
This little finger-shaped organ, often dismissed as an evolutionary leftover, is packed with immune cells.
It’s like a mini-fortress guarding our digestive system.
The appendix is rich in immune cells that have a primary function in detecting and removing pathogens.
But here’s the interesting part: the appendix also seems to be a haven for gut bacteria, those trillions of tiny organisms that play a big role in our health.
Recent studies have linked gut inflammation and changes in this gut microbiome to PD. And guess what?
The appendix seems to be right in the middle of all this action.
Could it be that this long-overlooked organ is a key player in the development of Parkinson’s?

Severe Infections
One study found that young adults who had their appendix removed (appendectomy) were more than twice as likely to be hospitalized with a severe infection caused by a type of Salmonella bacteria.
This finding suggests the appendix might help our bodies fight these bad bugs.
Appendectomy and the Microbiome
In another study, researchers analyzed bacterial and fungal diversity and composition in fecal samples from 30 individuals who had undergone appendectomy more than six months earlier.
The subjects were otherwise healthy. The scientists compared these individuals with 30 healthy individuals who had not undergone an appendectomy.
Appendectomy and the Microbiome Study Results
Analysis of these samples showed that the alpha diversity was comparable between the two groups overall but was lower among those who had undergone appendectomy less than two years before study entry than those who had undergone the procedure more than two years before.
The beta diversity differed between the groups but tended to shift over time in individuals who had undergone appendectomy toward that of individuals who had not.
The taxonomic analysis identified a lower level of several microbe types species and a higher abundance of others in the people who had undergone an appendectomy.
Gut fungal diversity was higher among people who had undergone appendectomy than among those who had not, and these alterations persisted over five years.
Analysis of interkingdom interactions indicated that interactions between bacteria and fungi were altered substantially after an appendectomy.
My Takeaway – Is the Appendix Useless?
Do you have these symptoms?
- Sudden pain begins around the belly button (and may shift to the lower right abdomen)
- Pain that worsens with walking, coughing, or making other jarring movements
- Nausea and vomiting
- Appetite loss
- Low-grade fever may rise as the illness worsens
- Diarrhea or constipation
- Abdominal bloating or gas
While surgery (appendectomy) has been the go-to solution for this condition, there might be a plot twist thanks to a powerful ally: antibiotics.
A careful assessment is crucial before any surgery, and recent research suggests antibiotics could potentially “fix” the problem instead.
On the other hand, the research findings remind me to take care of my gut microbiome.
Promoting Gut Microbiome Health
Our gut is a complex ecosystem teeming with trillions of tiny bacteria, both good and bad.
What we eat is huge in tipping the scales towards a healthy gut or a grumpy one.
Here’s the lowdown on gut-friendly foods and those best enjoyed in moderation:
Gut Bullies
- Sugar Rush Blues: Sugar is like candy for bad bacteria, leading to an overgrowth that can wreak havoc on your gut health.

- Processed Food Peril: Highly processed foods often lack fiber and nutrients, offering little nourishment for gut bacteria.
- Alcohol’s Aftereffect: While a glass of wine might seem relaxing, excessive alcohol consumption can disrupt the delicate balance of bacteria in your gut.
Gut BFFs
- Fiber Fiesta: Whole grains, fruits, and vegetables are packed with fiber, which acts like food for your good gut bacteria. Think of it as a probiotic buffet!
- Prebiotic Powerhouse: Onions, garlic, and fermented foods like yogurt and miso are rich in prebiotics, which help your good bacteria thrive.
- Rainbow on Your Plate: Eating various colorful fruits and vegetables provides diverse nutrients that benefit gut health.
The Key: Balance is Best
Don’t feel like you have to become a saint and swear off all your favorite treats!
For me, moderation is key.
Enjoy a sugary treat occasionally, but balance it with many gut-friendly choices.
Remember, a healthy gut is happy, which can contribute to a happier, healthier you.
Thank you for reading “Vindication for the Appendix: This ‘Useless’ Organ Finally Gets Its Day in Court.”




