Chemo Brain Fog: Blame it on the Gut?
Earlier this week, I met a lovely young woman who had recently completed chemotherapy for breast cancer.
She complained of treatment-related cognitive impairment — chemo fog — with some memory and thinking problems.
As a radiation oncologist, I often hear cancer survivors use the term “chemo brain” to describe the frustrating cognitive difficulties they experience during and after treatment.
I sometimes hear such complaints after radiation therapy or pills (endocrine therapy) that block estrogen.
While “chemo brain” is a widely recognized term, the exact causes of these cognitive problems remain elusive.

Now comes a possible explanation for chemotherapy-induced brain fog: the gut microbiome.
Let’s briefly examine chemobrain symptoms, risk factors, and new evidence pointing to the gut.
I’ll end with some tips about how you can optimize your microbiome.
Chemo Brain Symptoms
The manifestations of chemo brain can be diverse and often subtle, affecting various aspects of cognitive function.
Individuals may experience a heightened sense of disorganization, confusion, and difficulty concentrating.
Finding the right word can become challenging, as can learning new skills or multitasking effectively.
Many describe a pervasive feeling of mental fogginess, coupled with a shortened attention span and difficulties with short-term memory.
Completing routine tasks may take longer than usual, and problems with verbal and visual memory can further complicate daily life.
Chemo Brain Fog: Blame it on the Gut?
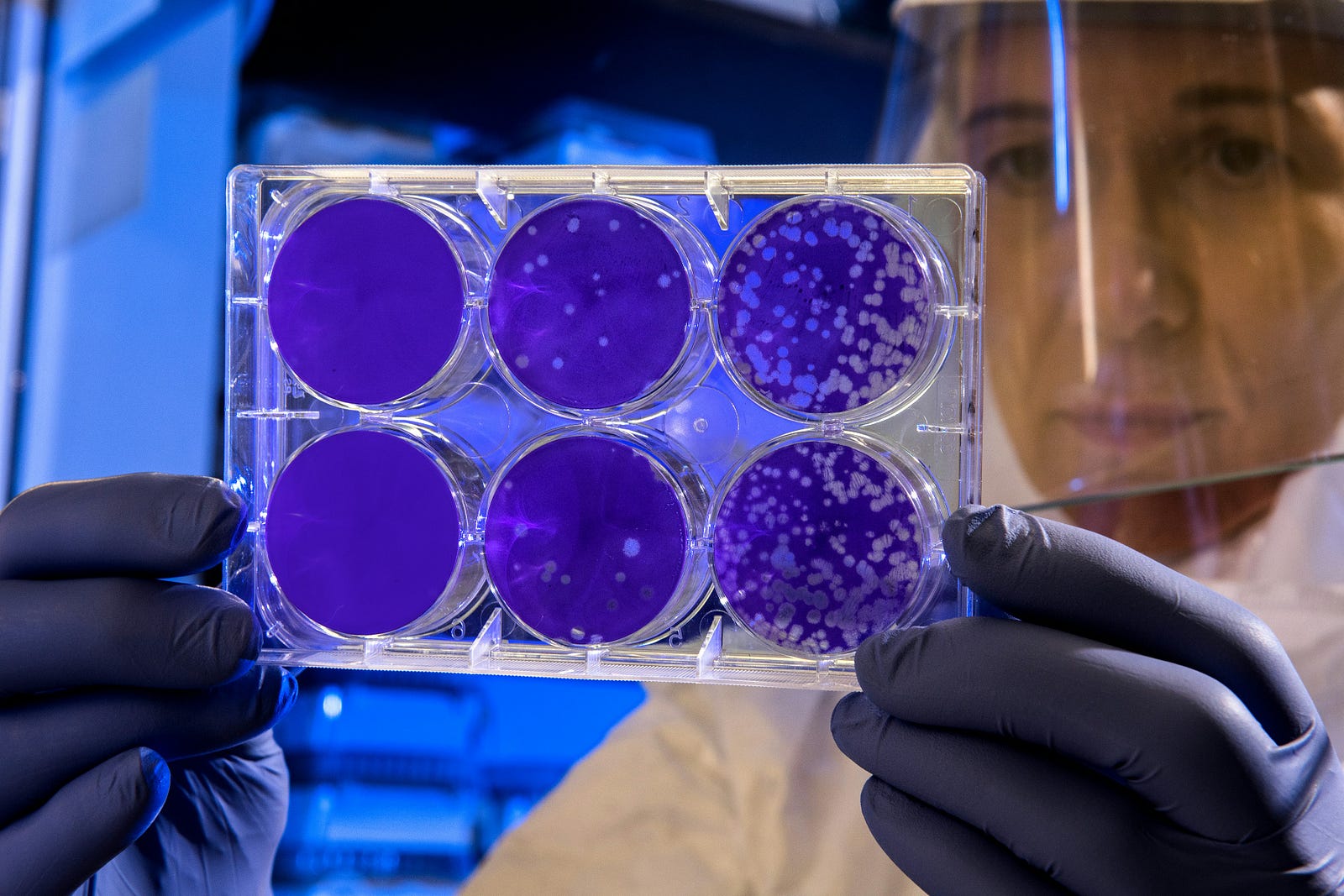
Researchers investigated the potential link between gut microbiome and cognitive function.

The Intelligut study followed 77 women with breast cancer over time.
Researchers collected fecal samples to analyze the gut microbiome.
They also obtained blood samples and conducted cognitive assessments before, during, and after chemotherapy.
This longitudinal design allowed for examining changes in the gut microbiome and cognitive function throughout treatment.
Study Details
Scientists conducted a comprehensive study involving women with breast cancer, visiting them at three critical time points during their treatment journey.
Their first visit occurred before the initiation of chemotherapy, during which we collected baseline measurements of their gut microbiome through fecal samples.
They also obtained blood samples to assess inflammatory immune markers and administered a battery of cognitive tests to establish baseline cognitive function.

More Study Details
The second visit coincided with the final chemotherapy infusion, during which researchers repeated the collection of fecal and blood samples and cognitive assessments to gauge any changes that may have occurred during treatment.
Finally, the authors conducted our third visit approximately three months after chemotherapy, collecting fecal and blood samples and performing cognitive tests.
This final visit allowed them to evaluate chemotherapy’s long-term impact on the gut microbiome and cognitive function.
Study Findings: Microbiome Matters
Researchers discovered some interesting findings.
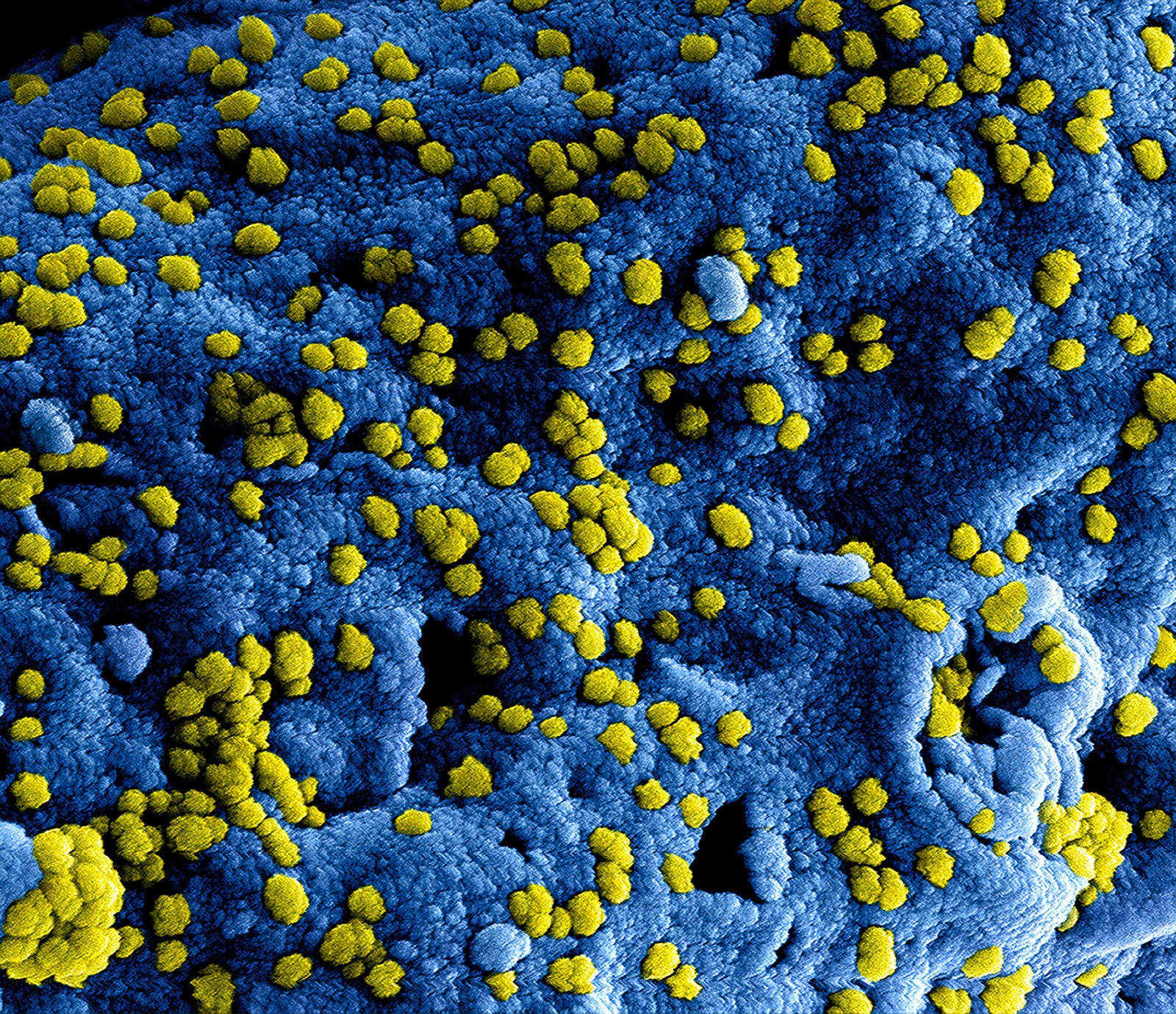
Chemotherapy-induced alterations in the gut microbiome’s community structure and elevated circulating tumor necrosis factor-alpha levels.
While study participants reported experiencing subjective cognitive decline during chemotherapy, the researchers found no direct link between these self-reported symptoms and changes in the gut microbiome or inflammatory markers.
However, a significant finding emerged:
Decreases in overall objective cognition were associated with a reduction in microbial diversity, independent of the influence of circulating inflammatory cytokines.
Implications – Chemo Brain Fog: Blame it on the Gut?
This observation suggests a potential role for gut microbiome diversity in cognitive function.
Further analysis revealed distinct taxonomic shifts within the gut microbiome of patients who experienced cognitive decline compared to those who did not.
These unique patterns of microbial abundance could offer valuable insights into the specific bacteria involved in cognitive impairment following chemotherapy.
Summary – Chemo Brain Fog: Blame it on the Gut?
Interestingly, the study revealed that while some patients experienced cognitive decline after chemotherapy, these effects were linked to changes in their gut microbiome rather than inflammation.
Despite observing inflammation related to gut microbiome alterations, it did not correlate with cognitive decline.
This observation suggests that the gut-brain axis may not primarily involve the immune system as a communication pathway in chemobrain.
Traditionally, the hypothesis has been that gut microbiome disruptions could trigger immune system activation, leading to cognitive problems through immune signaling.
However, the current study results challenge this notion; we should explore alternative gut-brain communication mechanisms.
Specifically, the study authors suspect that metabolites produced by the gut microbiome might play a crucial role.
These metabolites, such as short-chain fatty acids and bile acids, can enter the bloodstream and directly influence brain function.
Disruptions in the gut microbiome could alter the quantity and composition of these metabolites, potentially contributing to cognitive decline.
This study reminds me of how much more research we need into the complex interactions between the gut microbiome, metabolites, and brain health.
What About You and Me?
Are there any practical implications for you and me?
The study reminds me of the relationship between our microbiome and health.
The microbiome is associated with:
- Gut health
- Heart health
- Weight
- Blood sugar (and diabetes risk)
- Brain health

How Can You Improve Your Gut Microbiome?
Healthline offers these tips for improving your
To support a healthy gut microbiome and potentially mitigate the risk of chemo brain, consider incorporating the following dietary and lifestyle modifications:
- Embrace Dietary Diversity: Consume a wide variety of foods, particularly legumes, beans, and fruits, as they are rich in fiber and promote the growth of beneficial Bifidobacteria.
- Ferment for Gut Health: Include fermented foods like yogurt, sauerkraut, and kefir in your diet. These foods contain healthy bacteria, primarily Lactobacilli, which can help reduce harmful species in the gut.
- Limit Artificial Sweeteners: Avoid or minimize the consumption of artificial sweeteners like aspartame, as they may promote the growth of unhealthy bacteria and disrupt blood sugar levels.
- Prioritize Prebiotic Foods: Incorporate prebiotic-rich foods into your meals, such as artichokes, bananas, asparagus, oats, and apples. These foods nourish beneficial gut bacteria and promote their growth.
- Breastfeed for Optimal Gut Development: For infants, breastfeeding for at least six months plays a crucial role in establishing a healthy gut microbiome, particularly by fostering the growth of Bifidobacteria.
- Choose Whole Grains: Opt for whole grains over refined grains. They are packed with fiber and beneficial carbohydrates like beta-glucan, which gut bacteria digest to promote overall health.
- Explore Plant-Based Options: Consider incorporating more plant-based meals into your diet. Vegetarian diets can help reduce harmful bacteria and inflammation while lowering cholesterol levels.
- Indulge in Polyphenol-Rich Foods: Enjoy foods rich in polyphenols, like red wine, green tea, dark chocolate, olive oil, and whole grains. The microbiome breaks down these compounds to stimulate the growth of beneficial bacteria.
- Consider Probiotic Supplements: Probiotics, available in supplement form, can help restore a healthy gut microbiome after dysbiosis by repopulating it with beneficial microbes.
- Use Antibiotics Judiciously: Take antibiotics only when necessary. They can disrupt the delicate balance of the gut microbiome and potentially contribute to weight gain and antibiotic resistance.
Consuming a diverse array of high-fiber and fermented foods is a key strategy for maintaining a healthy microbiome and potentially reducing the risk of chemobrain.
How Does Your Gut Microbiome Impact Your Overall Health?
The gut microbiome refers to the trillions of bacteria, viruses, and fungi in your gut.www.healthline.com
Thank you for reading “Chemo Brain Fog: Blame it on the Gut?”




