Envision a future where a simple blood test, a painless swab, or a breathalyzer could unveil every hidden ailment within your body, ushering in a new era of proactive and personalized healthcare. The end of diagnostic guesswork?
I am a doctor who helps patients with cancer.
A tool like this could get my patients in earlier (or even allow them to dodge cancer).
There will be no more agonizing wait for results, endless referrals to specialists, and no more misdiagnoses and their devastating consequences.

Such a test could revolutionize healthcare, providing early and accurate diagnoses, reducing the need for multiple tests and referrals, and ultimately improving patient outcomes.
The quest for a diagnostic holy grail has captivated scientists and physicians for centuries.
Caveats
I know.
The rise and fall of Stanford graduate Elizabeth Holmes and her company Theranos — promising revolutionary blood-testing technology that was subsequently revealed as a fraud—is a cautionary tale about pursuing advanced medical diagnostics.

When the fledgling biotech company burst onto the scene, audaciously claiming to have developed a product capable of performing hundreds of medical tests in a doctor’s office using just a single drop of blood, it seemed unbelievable.
It turns out that the amazing technology Theranos talked about wasn’t even real.
The True Story Behind The Dropout and the Elizabeth Holmes Theranos Scandal
With a charismatic performance from Amanda Seyfried as Elizabeth Holmes, The Dropout examines the wild world of Silicon…time.com
They promised they could do all these medical tests with just a tiny drop of blood, but they couldn’t.
Their machines weren’t accurate at all.
So, a couple of years after they shut down their labs, the company’s leader, Elizabeth Holmes, and her partner in charge, Sunny Balwani, were charged with tricking people into lying about what their product could do.
/media/1baae84daa93caf75c0de30aed7aec89
A New Blood Test
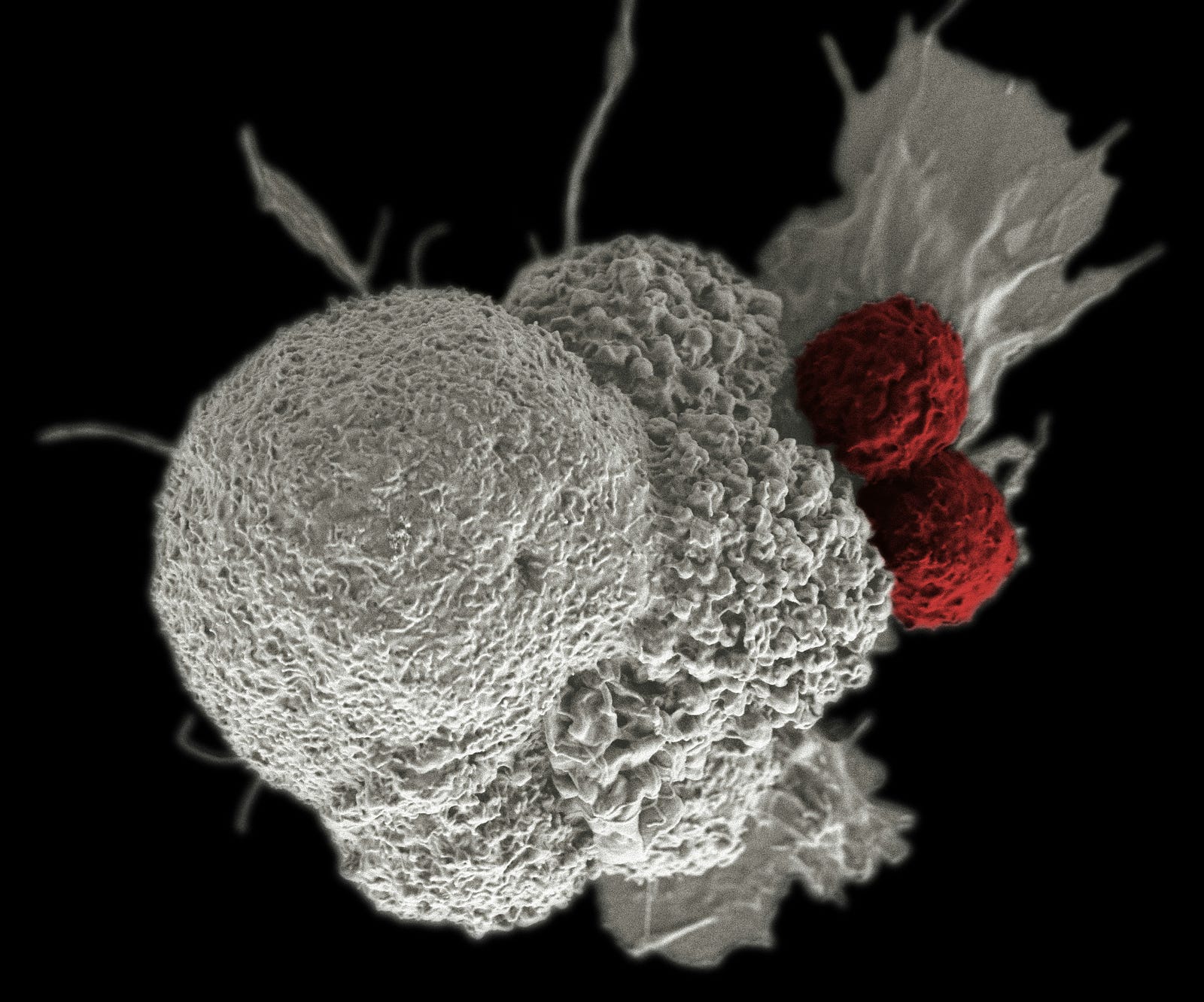
Today, fueled by advancements in genomics, proteomics (the large-scale study of proteins) plays a crucial role in developing a “one test to rule them all”.
Combined with artificial intelligence, we stand on the precipice of a revolution that could redefine healthcare as we know it.
In this essay, I will take you on a journey through the cutting-edge of medical diagnostics.
We will explore the technologies making the “one test to rule them all” a reality, examine the potential benefits and challenges of such a breakthrough, and ponder the ethical and societal implications of a world where disease detection is no longer a guessing game.
Challenges
The urgent need for rapid and widespread testing during the COVID-19 pandemic accelerated research and development into tests that could simultaneously detect multiple diseases.
The Siemens Advia 1800 machine, about the size of a minifridge, can run dozens of tests.
Technological challenges
Here’s the challenge: Can a company design an analyzer the size of a desktop that can run hundreds of tests?
Add another challenge: Do it on just a few drops of blood.
Is there a cap on how many tests a single blood sample can allow?
Some tests require chemical reactions that change the blood’s composition, rendering it unsuitable for additional analysis.
That’s why I didn’t believe Theranos’ claims.
A Chilling Effect: Investors Become Skeptical
The Verge reported, “When a Wall Street Journal investigation first revealed that Theranos couldn’t accomplish what it had promised, investors didn’t want to fund the projects.”
Improving Risk Prediction for Disease
Certainly, let’s break down the key aspects of your cohort study conducted within the UK Biobank Prospective Pivot Study (UKB-PPP):
- Plasma Proteomic Profiling: Researchers analyzed plasma samples, targeting 2,923 unique proteins via 2,941 assays.
- Prediction Models: Researchers developed models to predict the risk of 218 diseases. They built models on incident cases (new disease occurrences) arising within a 10-year follow-up period.
- Study Population: Primarily focused on a random subset of the UKB-PPP (41,931 individuals) for 193 diseases. They also included a consortium-selected subset to analyze an additional 25 diseases.
- Disease Definitions: Based on previously validated phenotypes, integrating data from diverse sources, including 1) primary care records, 2) hospital episode statistics, 3) cancer and death registries, and 4) UK Biobank health questionnaires (self-reported illnesses).
The investigators excluded those with diseases present at (or before) the baseline assessment and disallowed incident cases occurring within the first six months of follow-up.

Study Findings – The End of Diagnostic Guesswork?
Researchers published in the journal Nature Medicine.
The blood test could predict 67 major diseases, including cancer and dementia, up to 10 years early.
“We are extremely excited about the opportunity to identify new markers for screening and diagnosis from the thousands of proteins circulating and now measurable in human blood,” said lead author Claudia Langenberg, PhD, director of the Precision Healthcare University Research Institute (PHURI) at Queen Mary University of London.
Protein signatures offered opportunities to improve the detection and prognosis of many diseases.
Summary – The End of Diagnostic Guesswork?
Here are the key takeaways regarding the performance of the protein-based prediction models in comparison to other models:
- Sparse protein signatures: Using a limited set of the most important proteins (5 to 20) yielded better predictions than models based on basic clinical information for 67 diverse diseases.
- Protein versus clinical models with blood assays: Protein-based models outperformed clinical models incorporating blood assays for 52 of the 52 diseases studied.
- Protein vs. polygenic risk scores: Polygenic risk scores were available for 23 diseases, superior to clinical models (without blood assays) for seven diseases. However, proteins surpassed polygenic risk scores in predictive ability for all seven diseases except breast cancer.
Implications – The End of Diagnostic Guesswork?
These results strongly suggest the potential of protein-based models, particularly those utilizing sparse protein signatures, for enhancing disease prediction.
The protein-based models appear to outperform models based on basic clinical data and even those incorporating additional blood assays or polygenic risk scores (in most cases).
The study findings highlight the valuable information captured by proteomic profiling and its potential to contribute to improved risk assessment and potentially personalized medicine approaches.
While proteomics shows great promise, it is still a developing field.
One more thing:
Shocking Prediction: Cancer Cases Set to Skyrocket to 35 Million Globally by 2050
“AS THE WORLD AGES, CANCER CASES WILL RISE, hitting some countries like a tidal wave.”medium.com
Thank you for reading. “The End of Diagnostic Guesswork?“




